Procedures & Services:
- Laparoscopic Adrenal Surgery
- Laparoscopic Gall Bladder Surgery
- Single Incision Laparoscopic Surgery (SILS)
- Laparoscopic Anti-Reflux Surgery
- Laparoscopic Esophagus Surgery (Heller Procedure)
- Laparoscopic Gastric Resection
- Laparoscopic Inguinal Hernia Surgery
- Laparoscopic Abdominal Hernia Surgery
- Laparoscopic Colon Surgery
- Laparoscopic Spleen Surgery
- Laparoscopic Liver Surgery
- Laparoscopic Pancreas Surgery
- Laparoscopic Kidney Surgery
- Laparoscopic Appendix Surgery
- Laparoscopic Weight Loss Surgery
Laparoscopic Pancreatic Resection
The surgeons at University Surgeons Associates are experienced in using laparoscopic techniques to treat problems of the pancreas. They participate regularly in a multidisciplinary GI conference that reviews imaging, endoscopic findings and biopsies with the gastroenterologists, radiologists and pathologists. We utilize laparoscopic techniques to treat tumors in this region.
ABOUT CONVENTIONAL PANCREATIC SURGERY
Each year, a number surgical procedures are performed in the United States to treat diseases of the pancreas. Most of these are for pancreatic inflammation or tumors. Although surgery is not always a cure, it is often the best way to stop the spread of disease and alleviate symptoms.
Patients undergoing pancreatic surgery often face a long and difficult recovery because the traditional "open" procedures are highly invasive. In most cases, surgeons are required to make a long incision. Pancreatic operations are frequently lengthy and complex procedures. Surgery results in an average hospital stay of a week or more and usually 6 weeks of recovery.
WHAT IS THE PANCREAS?
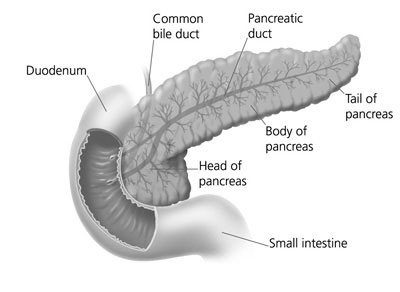
The pancreas is a gland located deep in the abdomen between the stomach and the spine (backbone). The liver, intestine, spleen and other organs surround the pancreas. The pancreas is about 6 inches long and is shaped like a flat pear. The widest part of the pancreas is the head, the middle section is the body, and the thinnest part is the tail.
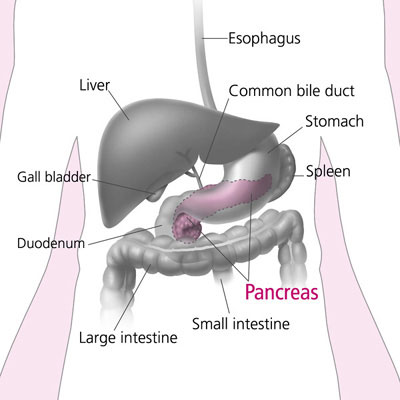
The pancreas makes insulin and other hormones. These hormones enter the bloodstream and travel throughout the body. They help the body use or store the energy that comes from food. For example, insulin helps control the amount of sugar in the blood. The pancreas also makes pancreatic juices. These juices contain enzymes that help digest food. The pancreas releases the juices into a system of ducts leading to the common bile duct. The common bile duct empties into the duodenum, the first section of the small intestine.
WHAT IS LAPAROSCOPIC PANCREATIC SURGERY?
A technique known as minimally invasive laparoscopic pancreatic surgery allows surgeons to perform many common pancreas procedures through small incisions. Depending on the type of procedure, patients may leave the hospital in a few days and return to normal activities more quickly than patients recovering from open surgery.
In most laparoscopic pancreatic resections, surgeons operate through 4 or 5 small openings (each about a quarter inch) while watching an enlarged image of the patient's internal organs on a television monitor. Sometimes the use of a hand port allows the surgeon to use a hand to assist with the surgery. In some cases, one of the small openings may be lengthened to 2 or 3 inches to complete the procedure and remove the portion of pancreas that has been resected.
WHAT ARE THE ADVANTAGES OF LAPAROSCOPIC PANCREATIC SURGERY?
Results may vary depending upon the type of procedure and patient's overall condition. Common advantages are:
- Less postoperative pain
- May shorten hospital stay
- May result in a faster return to solid-food diet
- May result in a quicker return of bowel function
- Quicker return to normal activity
- Improved cosmetic results
ARE YOU A CANDIDATE FOR LAPAROSCOPIC PANCREATIC SURGERY?
Although laparoscopic pancreatic surgery has many benefits, it may not be appropriate for some patients. Obtain a thorough medical evaluation by one of our surgeons, who in consultation with your primary care physician and/or gastroenterologist will advise if the technique is appropriate for you.
WHAT TO DO BEFORE SURGERY?
Advance tests...
Most diseases of the pancreas are diagnosed by imaging, endoscopic and blood tests. CT scans, ultrasound, MRI and nuclear medicine imaging are all useful in various pancreatic problems. A gastroscope is a soft, bendable tube about the thickness of the index finger which is inserted into the mouth and then advanced through the esophagus and stomach to the duodenum. Endoscopic retrograde pancreaticocholangiography (ERCP) allows visualization of the pancreatic duct and common bile duct through a specialized gastroscope. Biopsies and brushings of the ducts and pancreas can also be obtained. Endoscopic ultrasound evaluation is often helpful. A barium upper GI study is a special X-ray where a white “milk-shake fluid” is swallowed and pictures or videos of the esophagus, stomach and duodenum are taken. This test allows the surgeon to look inside of the upper gastrointestinal system and it may be useful. Prior to the operation, other blood tests, electrocardiogram (EKG) or a chest x-ray might be required.
Before surgery...
- Preoperative preparation includes blood work, medical evaluation, chest x-ray and an EKG depending on your age and medical condition.
- After your surgeon reviews with you the potential risks and benefits of the operation, you will need to provide written consent for surgery.
- Blood transfusion and/or blood products may be needed depending on your condition.
- It is recommended that you shower the night before or morning of the operation.
- Antibiotics by mouth are sometimes prescribed. Your surgeon or his/her staff will give you instructions.
- After midnight the night before the operation, you should not eat or drink anything except medications that your surgeon and/or anesthesiologist have told you to take with a sip of water the morning of surgery.
- Drugs such as aspirin, blood thinners, anti-inflammatory medications (arthritis medications) and Vitamin E will need to be stopped temporarily for several days to a week prior to surgery.
- Diet medication or St. John’s Wort should not be used for the two weeks prior to surgery.
- Quit smoking and arrange for any help you may need at home.
HOW IS LAPAROSCOPIC PANCREATIC SURGERY PERFORMED?
"Laparoscopic" surgery describes the techniques a surgeon uses to gain access to the internal surgery site.
Most laparoscopic pancreatic procedures start the same way. Using a cannula (a narrow tube-like instrument), the surgeon enters the abdomen. A laparoscope (a tiny telescope connected to a video camera) is inserted through the cannula, giving the surgeon a magnified view of the patient's internal organs on a television monitor. Several other cannulas are inserted to allow the surgeon to work inside and remove part of the pancreas. The entire procedure may be completed through the cannulas or by lengthening one of the small cannula incisions.
WHAT HAPPENS IF THE OPERATION CANNOT BE PERFORMED OR COMPLETED BY THE LAPAROSCOPIC METHOD?
In a number of patients the laparoscopic method cannot be performed. Factors that may increase the possibility of choosing or converting to the "open" procedure may include:
- Obesity
- A history of prior abdominal surgery causing dense scar tissue
- Inability to visualize organs
- Bleeding problems during the operation
- Large tumors
The decision to perform the open procedure is a judgment decision made by your surgeon either before or during the actual operation. When the surgeon feels that it is safest to convert the laparoscopic procedure to an open one, this is not a complication, but rather sound surgical judgment. The decision to convert to an open procedure is strictly based on patient safety.
WHAT SHOULD I EXPECT AFTER SURGERY?
After the operation, it is important to follow your doctor's instructions. Although many people feel better in a few days, remember that your body needs time to heal.
- You are encouraged to be out of bed the day after surgery and to walk. This will help diminish the soreness in your muscles.
- You will probably be able to get back to most of your normal activities in one to two weeks time. These activities include showering, driving, walking up stairs, working and engaging in sexual intercourse.
- Call and schedule a follow-up appointment within 2 weeks after your operation.
WHAT COMPLICATIONS CAN OCCUR?
These complications include:
- Bleeding
- Infection
- A leak of pancreatic fluid
- Injury to adjacent organs such as the small intestine or spleen
- Blood clots to the lungs.
It is important for you to recognize the early signs of possible complications. Contact your surgeon if you notice severe abdominal pain, fevers, chills, drainage or rectal bleeding.
WHEN TO CALL YOUR DOCTOR
Be sure to call your physician or surgeon if you develop any of the following:
- Persistent fever over 101 degrees F (39 C)
- Bleeding from the rectum
- Increasing abdominal swelling
- Pain that is not relieved by your medications
- Persistent nausea or vomiting
- Chills
- Persistent cough or shortness of breath
- Purulent drainage (pus) from any incision
- Redness surrounding any of your incisions that is worsening or getting bigger
- You are unable to eat or drink liquids

