Specializing in-
Pancreatic Surgery
The surgeons at University Surgeons Associates are experienced in using surgical techniques to treat problems of the pancreas. They participate regularly in the multidisciplinary GI conference that reviews imaging, endoscopic findings and biopsies with the gastroenterologists, radiologists and pathologists. We utilize laparoscopic and open techniques to treat tumors, cysts and inflammation in this region.
ABOUT CONVENTIONAL PANCREATIC SURGERY
Each year, a number surgical procedures are performed in the United States to treat diseases of the pancreas. Most of these are for pancreatic inflammation or tumors. Although surgery is not always a cure, it is often the best way to stop the spread of disease and alleviate symptoms. Cancer of the pancreas is diagnosed in more than 29,000 people every year. Pancreatic operations are frequently lengthy and complex procedures. Surgery results in an average hospital stay of a week or more.
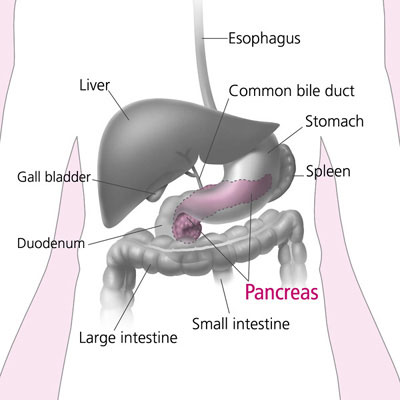
WHAT IS THE PANCREAS?
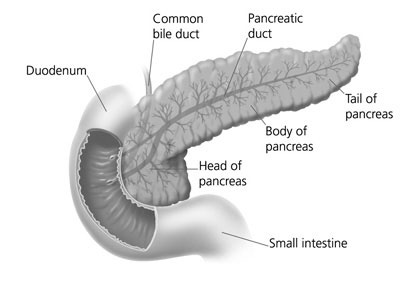
The pancreas is a gland located deep in the abdomen between the stomach and the spine (backbone). The liver, intestine, spleen and other organs surround the pancreas. The pancreas is about 6 inches long and is shaped like a flat pear. The widest part of the pancreas is the head, the middle section is the body, and the thinnest part is the tail.
The pancreas makes insulin and other hormones. These hormones enter the bloodstream and travel throughout the body. They help the body use or store the energy that comes from food. For example, insulin helps control the amount of sugar in the blood. The pancreas also makes pancreatic juices. These juices contain enzymes that help digest food. The pancreas releases the juices into a system of ducts leading to the common bile duct. The common bile duct empties into the duodenum, the first section of the small intestine.
WHAT TO DO BEFORE SURGERY?
Advance tests...
Most diseases of the pancreas are diagnosed by imaging, endoscopic and blood tests. CT scans, ultrasound, MRI and nuclear medicine imaging are all useful in various pancreatic problems. A gastroscope is a soft, bendable tube about the thickness of the index finger which is inserted into the mouth and then advanced through the esophagus and stomach to the duodenum. Endoscopic retrograde pancreaticocholangiography (ERCP) allows visualization of the pancreatic duct and common bile duct through a specialized gastroscope. Biopsies and brushings of the ducts and pancreas can also be obtained. Endoscopic ultrasound evaluation is often helpful. A barium upper GI study is a special X-ray where a white “milk-shake fluid” is swallowed and pictures or videos of the esophagus, stomach and duodenum are taken. This test allows the surgeon to get a picture of the upper gastrointestinal system and it may be useful. Prior to the operation, other blood tests, electrocardiogram (EKG) or a chest x-ray might be required.
Before surgery...
- Preoperative preparation includes blood work, medical evaluation, chest x-ray and an EKG depending on your age and medical condition.
- After your surgeon reviews with you the potential risks and benefits of the operation, you will need to provide written consent for surgery.
- Blood transfusion and/or blood products may be needed depending on your condition.
- It is recommended that you shower the night before or morning of the operation.
- Antibiotics by mouth are sometimes prescribed. Your surgeon or his/her staff will give you instructions.
- After midnight the night before the operation, you should not eat or drink anything except medications that your surgeon and/or anesthesiologist have told you to take with a sip of water the morning of surgery.
- Drugs such as aspirin, blood thinners, anti-inflammatory medications (arthritis medications) and Vitamin E will need to be stopped temporarily for several days to a week prior to surgery.
- Diet medication or St. John’s Wort should not be used for the two weeks prior to surgery.
- Quit smoking and arrange for any help you may need at home.
HOW IS PANCREATIC SURGERY PERFORMED?
Open pancreatic surgery requires an upper abdominal incision. Usually, the incision is across the upper abdomen or in the midline. Occasionally, a diagnostic laparoscopy is done to establish the diagnosis or prepare the area for the procedure. Often intraoperative ultrasound scanning is useful in performing these procedures. Endoscopy of the biliary ducts is sometimes required. The surgeons of University Surgeons Associates are skilled in these techniques and use them regularly. It is not unusual to place drains at the end of these procedures and sometimes these drains need to remain in place for prolonged periods of time.
WHAT SHOULD I EXPECT AFTER SURGERY?
After the operation, it is important to follow your doctor's instructions. Although many people feel better in a few days, remember that your body needs time to heal.
- You are encouraged to be out of bed the day after surgery and to walk. This will help diminish the soreness in your muscles.
- You will probably be able to get back to most of your normal activities in two to three weeks time. These activities include showering, driving, walking up stairs, light exercise and even working.
- No heavy lifting for six weeks after this type of surgery.
- Call and schedule a follow-up appointment within 2 weeks after your operation.
WHAT COMPLICATIONS CAN OCCUR?
These complications include:
- Bleeding
- Infection
- A leak of pancreatic fluid
- Injury to adjacent organs such as the small intestine or spleen
- Blood clots to the lungs.
It is important for you to recognize the early signs of possible complications. Contact your surgeon if you notice severe abdominal pain, fevers, chills, drainage or rectal bleeding.
WHEN TO CALL YOUR DOCTOR
Be sure to call your physician or surgeon if you develop any of the following:
- Persistent fever over 101 degrees F (39 C)
- Bleeding from the rectum
- Increasing abdominal swelling
- Pain that is not relieved by your medications
- Persistent nausea or vomiting
- Chills
- Persistent cough or shortness of breath
- Purulent drainage (pus) from any incision
- Redness surrounding any of your incisions that is worsening or getting bigger
- You are unable to eat or drink liquids

