Specializing in-
Hepatobiliary Surgery
The surgeons at University Surgeons Associates are experienced in using surgical techniques to treat problems in the liver and bile ducts. They participate regularly in the UT Medical Center’s multidisciplinary GI conference that reviews imaging, endoscopic findings and biopsies with the gastroenterologists, radiologists and pathologists. We utilize laparoscopic and open approaches to treat and/or resect cysts, tumors and ductal problems in this region.
ABOUT CONVENTIONAL LIVER SURGERY
Each year, a number surgical procedures are performed in the United States to treat diseases of the liver. Most of these are for cysts or tumors. Some of these are for problems of the bile ducts. Although surgery is not always a cure, it is often the best way to stop the spread of disease and alleviate symptoms. The operations are often complex and lengthy. Surgery results in an average hospital stay of a week or more.
WHAT IS THE LIVER?
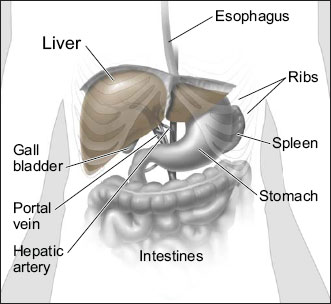
The liver is the largest organ inside your abdomen. The majority of the liver resides in the right upper abdomen, under the ribs, with the left lobe extanding to the left of the midline. The upper surface of the liver rests against the diaphragm. The liver gets its supply of blood from two vessels. Most of its blood comes from the hepatic portal vein. The rest comes from the hepatic artery. The liver does important work to keep you healthy:
- Detoxifies harmful substances from the blood.
- Produces enzymes and bile that help digest food.
- Converts food into substances needed for life and growth.
WHAT TO DO BEFORE SURGERY?
Advance tests...
Most diseases of the liver are diagnosed by imaging techniques or blood work. CT scans, ultrasound, MRI and nuclear medicine imaging are all useful in various liver problems. Sometimes an endoscopic ultrasound evaluation is helpful. Liver enzyme tests and special blood markers for liver diseases are often diagnostic. Prior to the operation, other blood tests, electrocardiogram (EKG) or a chest x-ray might be required.
Before surgery...
- Preoperative preparation includes blood work, medical evaluation, chest x-ray and an EKG depending on your age and medical condition.
- After your surgeon reviews with you the potential risks and benefits of the operation, you will need to provide written consent for surgery.
- Blood transfusion and/or blood products may be needed depending on your condition.
- It is recommended that you shower the night before or morning of the operation.
- Antibiotics by mouth are sometimes prescribed. Your surgeon or his/her staff will give you instructions.
- After midnight the night before the operation, you should not eat or drink anything except medications that your surgeon and/or anesthesiologist have told you to take with a sip of water the morning of surgery.
- Drugs such as aspirin, blood thinners, anti-inflammatory medications (arthritis medications) and Vitamin E will need to be stopped temporarily for several days to a week prior to surgery.
- Diet medication or St. John’s Wort should not be used for the two weeks prior to surgery.
- Quit smoking and arrange for any help you may need at home.
HOW IS HEPATIC SURGERY PERFORMED?
Open liver surgery or surgery on the bile ducts requires an upper abdominal incision. Usually, the incision is in the right upper abdomen or across the upper abdomen. Occasionally, a diagnostic laparoscopy is done to establish the diagnosis or prepare the area for the procedure. Often intraoperative ultrasound scanning is useful in performing these procedures. Endoscopy of the biliary ducts is sometimes required. The surgeons of University Surgeons Associates are skilled in these techniques and use them regularly. It is not unusual to place drains at the end of these procedures and sometimes these drains need to remain in place for prolonged periods of time. The liver is very vascular and therefore transfusion is sometimes required in these procedures.
WHAT SHOULD I EXPECT AFTER SURGERY?
After the operation, it is important to follow your doctor's instructions. Although many people feel better in a few days, remember that your body needs time to heal.
- You are encouraged to be out of bed the day after surgery and to walk. This will help diminish the soreness in your muscles.
- You will probably be able to get back to most of your normal activities in two to three weeks time. These activities include showering, driving, walking up stairs, light exercise and even working.
- No heavy lifting for six weeks after this type of surgery.
- Call and schedule a follow-up appointment within 2 weeks after your operation.
WHAT COMPLICATIONS CAN OCCUR?
These complications include:
- Bleeding
- Infection
- A bile leak where the liver or bile ducts were closed
- Injury to adjacent organs such as the small intestine, spleen, or pancreas
- Blood clots to the lungs
It is important for you to recognize the early signs of possible complications. Contact your surgeon if you notice severe abdominal pain, fevers, chills, or rectal bleeding.
WHEN TO CALL YOUR DOCTOR
Be sure to call your physician or surgeon if you develop any of the following:
- Persistent fever over 101 degrees F (39 C)
- Bleeding from the rectum
- Increasing abdominal swelling
- Pain that is not relieved by your medications
- Persistent nausea or vomiting
- Jaundice
- Chills
- Persistent cough or shortness of breath
- Purulent drainage (pus) from any incision
- Redness surrounding any of your incisions that is worsening or getting bigger
- You are unable to eat or drink liquids

