Specializing in-
Robotic Gastric Bypass
Weight loss surgery is a big and often complex decision. The multidisciplinary team at University Surgeons Associates takes a comprehensive approach to weight loss to help each patient find the best long-term outcome. We strive to offer the best possible opportunity to succeed in the fight against obesity and the illnesses associated with it. Robotic gastric bypass surgery is one option for people who are severely overweight.
WHAT IS SEVERE OBESITY?
Severe obesity, sometimes known as "morbid obesity", is defined as being approximately 100 pounds (45.5 kg) or 100% above ideal body weight. This is determined according to the Metropolitan Life Insurance Company height and weight tables. Between 3-5% of the United States adult population has severe obesity. This condition is associated with the development of life-threatening complications such as hypertension, diabetes and coronary artery disease, to name a few.
Numerous therapeutic approaches to this problem have been advocated, including low calorie diets, medication, behavioral modification and exercise therapy. However, the only treatment proven to be effective in long-term management of morbid obesity is surgical intervention.
WHAT CAUSES SEVERE OBESITY?
The cause of severe obesity is poorly understood. There are probably many factors involved. In obese persons, the set point of stored energy is too high. This altered set point may result from a low metabolism with low energy expenditure, excessive caloric intake, or a combination of the above. There is scientific data that suggests obesity may be an inherited characteristic.
Severe obesity is most likely a result of a combination of genetic, psychosocial, environmental, social and cultural influences that interact resulting in the complex disorder of both appetite regulation and energy metabolism. Severe obesity does not appear to be a simple lack of self-control by the patient.
WHAT ARE THE TREATMENT OPTIONS?
MEDICAL TREATMENT
In 1991, the National Institutes of Health Conference concluded that non-surgical methods of weight loss for patients with severe obesity, except in rare instances, are not effective over long periods of time. It was shown that nearly all participants in any non-surgical weight-loss program for severe obesity regained their lost weight within 5 years. Although prescriptions and non-prescription medications are available to induce weight loss, there does not appear to be a role for long-term medical therapy in the management of morbid obesity. Medications that reduce appetite can result in 11 to 22 pound weight reduction. However, weight gain is rapid once medication is withdrawn. Various professional weight loss programs use behavior modification techniques in conjunction with low caloric diets and increased physical activity. Weight loss of one to two pounds per week has been reported, but nearly all the weight loss is regained after 5 years.
SURGICAL TREATMENT
A number of weight loss operations have been devised over the last 40-50 years. The operations recognized by most surgeons include: vertical banded gastroplasty, gastric banding (adjustable or non-adjustable), Roux-en-Y gastric bypass, and malabsorbtion procedures (biliopancreatic diversion, duodenal switch). Choosing between the different operative procedures involves the consideration of the unique needs of each patient.
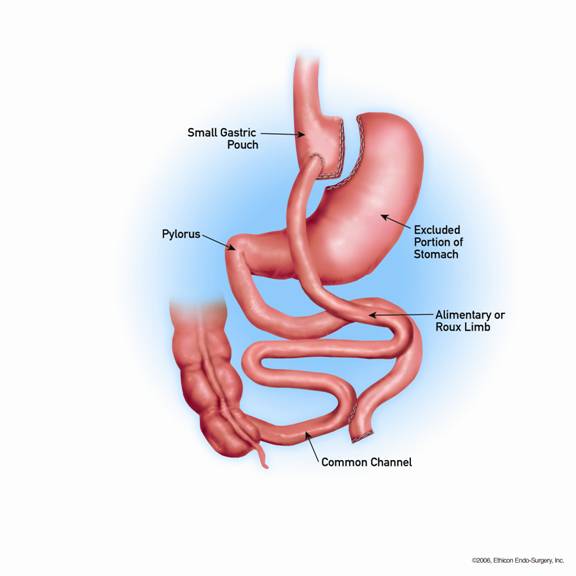
The gastric bypass procedure involves dividing the stomach and forming a small gastric pouch. The new gastric pouch is connected to varying lengths of your own small intestine constructed into a Y-shaped limb (Roux-en-Y gastric bypass).
WHAT ARE THE ADVANTAGES OF THE ROBOTIC GASTRIC BYPASS SURGERY?
Advantages of the laparoscopic approach include:
- Reduced post-operative pain
- Shorter hospital stay
- Faster return to work
- Improved cosmesis
- The use of wristed instruments that bend and rotate greater than the human hand allowing for your surgeon to operate with enhanced precision and control
WHO SHOULD BE CONSIDERED FOR ROBOTIC GASTRIC BYPASS SURGERY?
The following guidelines for selecting patients for obesity surgery were established by the National Institute of Health:
- Patients should exceed ideal body weight by approximately 100 pounds (45.5 kg) or 100% above ideals body weight.
- Patients should have no known metabolic (chemical breakdown of food into energy) or endocrine (hormone) causes for the morbid obesity.
- Patients should have an objectively measurable complication (physical, psychological, social, or economic) that might benefit from weight reduction. This includes hypertension (high blood pressure), diabetes (too much sugar in the blood), heart disease, breathing problems or lung disease, sleep apnea (snoring) and arthritis, just to name a few.
- The patient should understand the full importance of the proposed surgical procedure including suspected risks and complications.
- The patient should be willing to be observed and followed by a medical professional for many years.
- The patient should have attempted weight reduction using medical treatment without success.
- In some instances, a patient who is not quite 100 pounds or 100% above the ideal body weight is a candidate for surgical intervention. This patient should have a significant medical problem(s) that could benefit from weight reduction.
WHAT PREPARATION IS REQUIRED?
- A thorough medical evaluation to determine if you are a candidate for robotic obesity surgery by your physician.
- Supplemental diagnostic tests may be necessary, including a nutritional evaluation.
- A psychiatric or psychological evaluation may be required to determine the patient's ability to adjust to changes after the operation.
- Consultation from specialists, such as cardiologist, pulmonologist or endocrinologist may be needed depending on your own specific medical condition. Continued participation in Obesity Support Group is encouraged
- A written consent for surgery will be needed after the surgeon reviews the potential risks and benefits of the operation.
- The day prior to surgery, you will begin a clear liquid diet.
- Blood transfusion and/or blood products such as platelets may be needed depending on your condition.
- Your surgeon may request that you completely empty your colon and cleanse your intestines prior to surgery.
- It is recommended that you shower the night before or morning of the operation.
- After midnight the night before the operation, you should not eat or drink anything except medications that your surgeon has told you are permissible to take with a sip of water the morning of surgery.
- Drugs such as aspirin, blood thinners, anti-inflammatory medications (arthritis medications) and Vitamin E will need to be stopped temporarily for several days to a week prior to surgery.
- Diet medication or St. John's Wort should not be used for the two weeks prior to surgery.
- Quit smoking and arrange for any help you may need at home.
WHAT HAPPENS IF THE OPERATION CANNOT BE PERFORMED BY THE ROBOTIC METHOD?
In a small number of patients the robotic method cannot be performed. Factors that may increase the possibility of choosing or converting to the "open" procedure may include a history of prior abdominal surgery causing dense scar tissue, inability to visualize organs or bleeding problems during the operation.
The decision to perform the open procedure is a judgment decision made by your surgeon either before or during the actual operation. When the surgeon feels that it is safest to convert the robotic procedure to an open one, this is not a complication, but rather sound surgical judgment. The decision to convert to an open procedure is strictly based on patient safety.
WHAT SHOULD I EXPECT THE DAY OF SURGERY?
- You will arrive at the hospital the morning of the operation.
- Preparation before surgery often includes changing into a hospital gown.
- A qualified medical staff member will place a small needle/catheter (IV) in your vein to dispense medication during your surgery.
- Often pre-operative medications are necessary.
- You will meet the anesthesiologist and discuss the anesthesia.
- You will be under general anesthesia (asleep) during the operation, which may last for several hours.
- Following the operation you will be sent to the recovery room until you are fully awake. Then you will be sent to your hospital room.
- Most patients stay in the hospital the night of surgery and may require additional hospital days to recover from the surgery.
WHAT ARE THE EXPECTED RESULTS AFTER ROBOTIC GASTRIC BYPASS SURGERY?
WEIGHT LOSS
The success rate for weight loss is typically a 60% loss of excess body weight. Weight loss generally continues for 18-24 months after surgery. Some weight gain is common about two to five years after surgery.
EFFECT OF SURGERY ON ASSOCIATED MEDICAL CONDITIONS
Weight reduction surgery has been reported to improve conditions such as sleep apnea, diabetes, high blood pressure and high cholesterol. Many patients report an improvement in mood and other aspects of psychosocial functioning after surgery. Because the robotic approach is performed in a similar manner to the open approach, the long-term results appear to be as effective.
WHAT COMPLICATIONS CAN OCCUR?
Although the operation is considered safe, complications may occur as they may occur with any major operation.
The immediate operative death rate for any of the robotic obesity procedures is relatively low in the reported case series (less than 2%). On the other hand, complications such as wound infections, wound breakdown, abscess, leaks from staple-line breakdown, perforation of the bowel, bowel obstruction, marginal ulcers, pulmonary problems and blood clots in the legs may be as high as 10% or more. In the post-operative period other problems may arise that may require more surgery. These problems include pouch dilatation, persistent vomiting, heartburn or failure to lose weight. In a rare individual, reversal of the operation is necessary due to a complication of surgery. Complication rates with secondary surgery are higher than after the first operation.
Gallstones are a common finding in the obese patient. Symptoms from these gallstones are a common occurrence with weight loss. Many physicians either treat patients with bile lowering medication or recommend gallbladder removal at the time of the operation. This should be discussed with your surgeon and physician.
After gastric bypass, nutritional deficiencies such as Vitamin B-12, folate, and iron may occur. Taking necessary vitamin and nutrient supplements can generally prevent them. Another potential result of gastric bypass is "Dumping Syndrome". Abdominal pain, cramping, sweating, and diarrhea characterize dumping Syndrome after eating drinks and foods that are high in sugar. Avoiding high sugar foods can prevent these symptoms.
Following obesity surgery, patients must re-orient themselves and adjust to the effect of a changing figure. Women who become pregnant after any of these surgical procedures need special attention from their doctors and clinical care team.
As with any operation, there is a risk of complication. In general, complication rates of the robotic and laparoscopic approaches are equal to or less than the conventional, open operations.
WHAT TO EXPECT AFTER SURGERY
You will usually be in the hospital 1 to 3 days after a robotic procedure. You may have a tube in your stomach and not be permitted to eat or drink anything until it is removed. You should be out of bed, sitting in a chair the night of surgery and walking by the following day. You will need to participate in breathing exercises. You will receive pain medication when you need it.
On the first of second day after surgery you may have an X-ray of your stomach. The X-ray is a way for the surgeon to know if the stapling of the stomach is okay before beginning to allow you to eat. If no leakage or blockage is seen (the usual case) then you will be permitted to have one ounce of liquids every hour. The volume of liquid you drink will be gradually increased. Some surgeons allow you to eat baby food or a "puree" type of food. You will remain on a liquid or puree diet until your doctor evaluates you approximately 1-2 weeks after you return home.
Patients are encouraged to walk and engage in light activity. It is important to continue the breathing exercises while at home after surgery. Pain after robotic surgery is generally mild although some patients may require pain medication. At the first follow-up visit the surgeon will discuss with you any dietary changes.
After the operation, it is important to follow your doctor's instructions. Although many people feel better in just a few days, remember that your body needs time to heal. You will probably be able to get back to most of your normal activities in one to two week's time.
You should call and schedule a follow-up appointment within 2 weeks after your operation.
WHEN TO CALL YOUR DOCTOR
Be sure to call your doctor if you develop any of the following:
- Persistent fever over 101F (39 C)
- Bleeding
- Increased abdominal swelling or pain
- Persistent nausea or vomiting
- Chills
- Persistent cough and shortness of breath
- Difficulty swallowing that does not go away within a few weeks
- Drainage from any incision
- Calf swelling or leg tenderness

